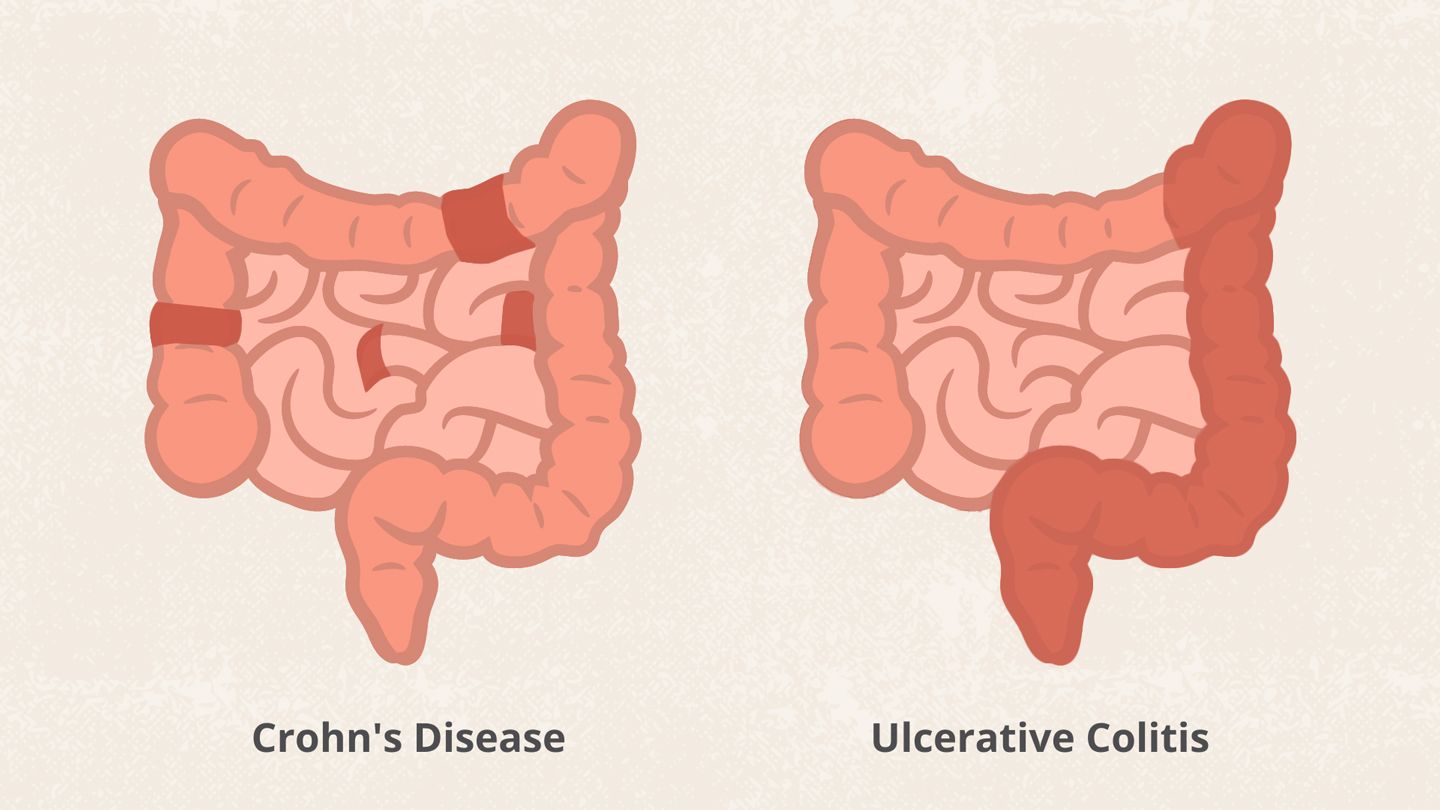
Understanding Crohn’s Disease: Symptoms, Causes, and Treatment Options Crohn’s disease is a chronic inflammatory condition that primarily affects the gastrointestinal tract. It is a type of inflammatory bowel disease (IBD), along with ulcerative colitis. While the exact cause of Crohn’s disease remains unknown, it is believed to involve a combination of genetic, environmental, and immune factors. This article aims to explore the various aspects of Crohn’s disease, including its symptoms, causes, diagnosis, and treatment options.
Symptoms of Crohn’s Disease
Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus. The symptoms of Crohn’s disease can vary widely among individuals and may change over time. Common symptoms include:
- Abdominal Pain: Persistent or recurring abdominal pain and cramping are hallmark symptoms of Crohn’s disease. The pain is often located in the lower right area of the abdomen but can occur anywhere in the abdomen.
- Diarrhea: Chronic diarrhea is a common symptom of Crohn’s disease. It may be accompanied by blood or mucus in the stool.
- Rectal Bleeding: Bleeding from the rectum can occur due to inflammation or ulceration in the intestinal lining.
- Weight Loss: Loss of appetite, nausea, and vomiting can lead to unintended weight loss in individuals with Crohn’s disease.
- Fatigue: Chronic inflammation and nutrient malabsorption can cause fatigue and weakness.
- Other Symptoms: Additional symptoms may include fever, joint pain, skin rashes, and eye inflammation.
Causes of Crohn’s Disease
The exact cause of Crohn’s disease is not fully understood, but it is believed to involve a complex interplay of genetic, environmental, and immune factors. Some potential causes and risk factors include:
- Genetics: Family history plays a significant role in the development of Crohn’s disease. Individuals with a close relative, such as a parent or sibling, with Crohn’s disease are at a higher risk of developing the condition themselves.
- Immune System Dysfunction: Crohn’s disease is characterized by an abnormal immune response in which the immune system mistakenly attacks healthy cells in the digestive tract, leading to inflammation.
- Environmental Factors: Environmental factors such as diet, smoking, and exposure to certain infections or pollutants may contribute to the development or exacerbation of Crohn’s disease.
- Microbiome Imbalance: Alterations in the gut microbiome, the community of microorganisms that inhabit the digestive tract, may play a role in the development of Crohn’s disease.
Diagnosis of Crohn’s Disease
Diagnosing Crohn’s disease typically involves a combination of medical history evaluation, physical examination, laboratory tests, imaging studies, and endoscopic procedures. Common diagnostic tests include:
- Blood Tests: Blood tests may be performed to assess inflammation levels, anemia, and nutritional deficiencies.
- Stool Tests: Stool samples may be analyzed for signs of infection, inflammation, or blood.
- Colonoscopy: During a colonoscopy, a flexible tube with a camera is inserted into the rectum to examine the entire colon and terminal ileum. Biopsies may be taken for further analysis.
- Imaging Studies: X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI), or ultrasound may be used to visualize the gastrointestinal tract and assess for signs of inflammation or complications.
Treatment Options for Crohn’s Disease
Treatment for Crohn’s disease aims to reduce inflammation, control symptoms, and prevent complications. The treatment approach may vary depending on the severity and location of the disease, as well as individual patient factors. Common treatment options include:
- Medications: Anti-inflammatory drugs, immunosuppressants, corticosteroids, antibiotics, and biologic therapies may be prescribed to reduce inflammation and suppress the immune system.
- Nutritional Therapy: Some individuals may benefit from nutritional supplementation or specialized diets to manage symptoms and promote healing of the intestinal lining.
- Lifestyle Modifications: Adopting a healthy lifestyle, including regular exercise, stress management, and smoking cessation, may help reduce symptoms and improve overall well-being.
- Surgery: In cases of severe or complications such as strictures, fistulas, or intestinal obstructions, surgery may be necessary to remove damaged portions of the intestine or alleviate blockages.
- Supportive Care: Supportive therapies such as counseling, support groups, and dietary counseling can help individuals cope with the physical and emotional challenges of living with Crohn’s disease.
Conclusion
Crohn’s disease is a complex and chronic inflammatory condition that can significantly impact the quality of life of affected individuals. While there is currently no cure for Crohn’s disease, with proper management and treatment, many people with the condition are able to achieve long-term remission and lead fulfilling lives.
Early diagnosis, ongoing medical care, and a multidisciplinary approach involving healthcare providers from various specialties are essential for effectively managing Crohn’s disease and minimizing its impact on patients’ lives. Further research into the underlying mechanisms of Crohn’s disease is needed to develop more targeted and personalized treatment strategies in the future.